Dental School Expands Treatment Services for Obstructive Sleep Apnea
January 31, 2020
Ann Arbor, Mich. - The School of Dentistry is expanding its resources for the treatment of patients with obstructive sleep apnea.
The condition causes breathing to repeatedly stop and start during sleep. It occurs when a person’s throat muscles intermittently relax and block the airway during sleep. It is a potentially serious disorder that has been linked to health issues such as cardiovascular disease, atrial fibrillation, heart attack, stroke and diabetes. Snoring is sometimes an indication of the condition.
The school’s faculty have been providing care to patients with obstructive sleep apnea for more than 15 years at the Dental Faculty Associates practice at the School of Dentistry and at the Hospital Dentistry Clinic within the University of Michigan Health System. This service is now being expanded into the Prosthodontic Faculty Clinic at the dental school as well as the Orofacial Pain Clinic, which is coordinated by the Department of Oral and Maxillofacial Surgery/Hospital Dentistry Department and located at the dental school’s Community Dental Center in downtown Ann Arbor.
Faculty members who are diplomates of the American Academy of Dental Sleep Medicine or qualified providers conduct treatment in collaboration with patients’ primary care physicians, sleep physicians and other health care professionals.
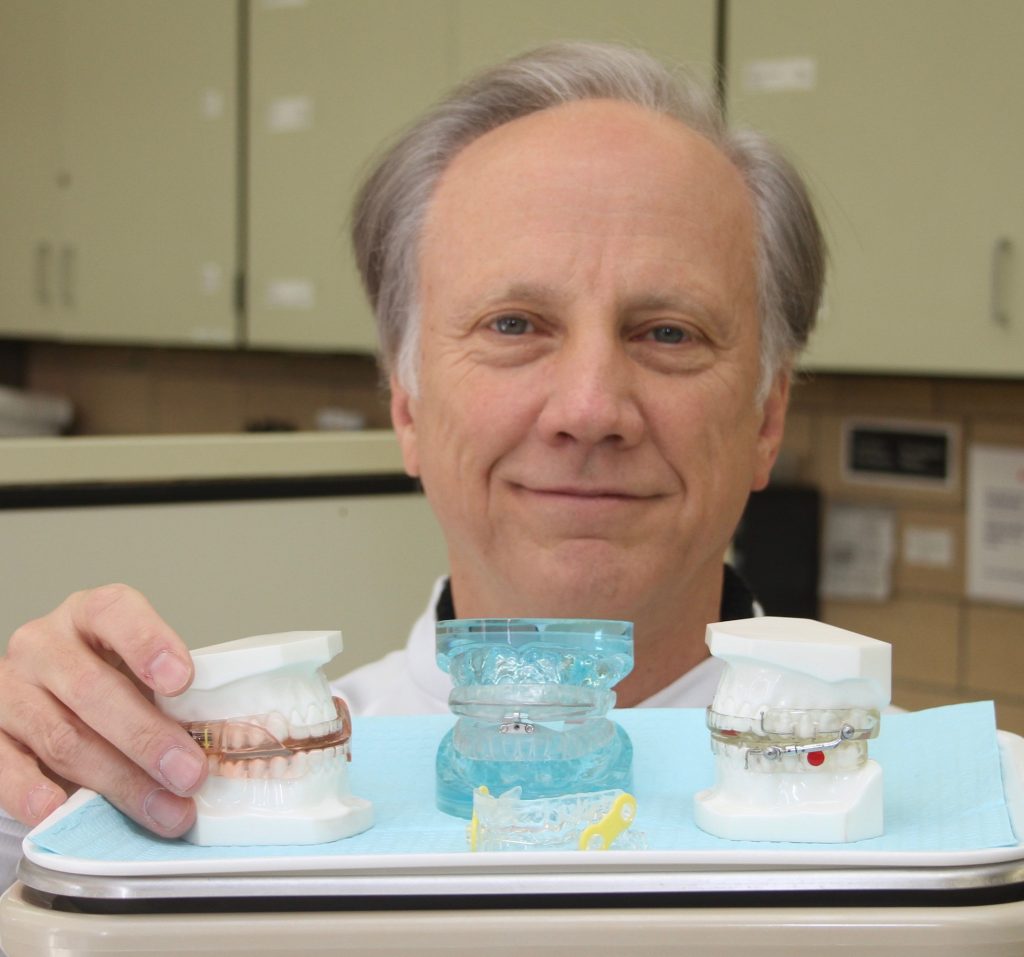
Dr. Geoffrey Gerstner with several types of oral appliances used in the treatment of obstructive sleep apnea.
The dental school’s services for treating obstructive sleep apnea, also known as OSA, are centered on oral appliance therapy. An oral appliance is a custom-fit device, similar to a sports mouth guard or orthodontic retainer, that is worn in the mouth as the patient sleeps overnight. The appliance is an effective treatment that prevents the airway from collapsing by moving the lower jaw forward.
Oral appliances are an alternative to the commonly used therapy called CPAP, an acronym for continuous positive airway pressure. Patients using CPAP machines wear a mask while they sleep and receive a continuous supply of air pumped to the mask through flexible tubing. It is an effective treatment for many people, but some are unable to tolerate or maintain the procedure on a regular basis. For those patients, oral appliances can be an effective alternative.
The dental school’s Dental Sleep Apnea Group accepts patients who are referred by a doctor and who have had a diagnostic sleep study. The dentist conducts a thorough examination to determine the best treatment options and proper oral appliance for the unique aspects of each patient’s mouth, jaw and upper airway structure.
Dr. Lawrence Ashman, clinical assistant professor in the Department of Oral and Maxillofacial Surgery/Hospital Dentistry, is the director of the apnea group at the Orofacial Pain Clinic. The group also includes Drs. Elizabeth Hatfield and Kristine Phillips, who are residents in the Temporomandibular Disorders and Orofacial Pain Residency Program.
Dental school faculty members Drs. Geoffrey Gerstner and Daniela Mendonca are co-directors of the apnea group at the Prosthodontic Faculty Clinic, which also includes Drs. Berna Saglik, Gustavo Mendonca, Elliot Hill and Marianella Sierraalta. Two dentists in private practice, Dr. Regina M Dailey and Dr. Earl Bogrow, also an adjunct faculty member, are special consultants.
Gerstner, an associate professor in the Department of Biologic and Materials Sciences & Prosthodontics, said OSA may affect as many as one in five people, according to various studies. Treating the condition is important because the quality of sleep a person gets has a significant impact on overall health and well-being.
Designing the proper oral appliance for patients depends on the unique aspects of each patient’s oral anatomy. Dentists use examinations, imaging and impressions of the patient’s mouth to create an oral appliance, much like how a denture is made. The impression is sent to a lab that makes the appliance, which is then fitted by the dentist. The four basic types of appliances have various functions, but most are related to moving the lower jaw forward in order to help open the airway in the patient’s throat while they sleep. Appliances are made from acrylic, plastic or nylon, with plastic or metal connections.
“We decide which design patients are going to use based on a case-by-case basis,” Gerstner said. “Some people grind their teeth at night, or their mouths may be small, or they may have lost their teeth. There are many other factors, so we make the oral appliances for each individual depending on their particular symptoms and mouth structure.”
As the dental school expands its OSA treatment services, local physicians are being contacted to make them aware of the Dental Sleep Apnea Group as a source for referrals.
The dental school’s sleep apnea initiative is being coordinated within the Department of Biologic and Materials Sciences & Prosthodontics. Dr. Jan Hu, the department chairman, said the dental faculty’s expertise in treating OSA is an excellent resource that fits well with local doctors, dentists and other health professionals treating apnea. “With the specialized training that our faculty members have in this area, we look forward to being a key part of the treatment network for local patients,” Hu said. “This is a growing area in healthcare and an example of how dental and medical issues are directly related to the overall health of patients.”
The faculty are also incorporating their OSA training into courses for dental students. A few hours of instruction are already part of the curriculum with more coursework planned for the future, Gerstner said.
Dr. Ashman’s group is located at Orofacial Pain Clinic at the Community Dental Center at 406 N. Ashley St. in Ann Arbor and can be reached at 734-998-6320. Patients who are referred to the dental school are managed at the Prosthodontic Faculty Clinic, which can be reached by calling 734-763-3326. More information is also available on the Obstructive Sleep Apnea Clinic web page on the dental school’s website.